Diabetes is a chronic metabolic disease characterized by an increase in blood glucose level (sugar, so glycemia) due to a lack or biological inefficiency of insulin, the hormone which controls glycemia and is produced by pancreas.
Diabetes is not a contagious disease: living with a diabetic person does not make you diabetic! Diabetes is not a hereditary disease: this means that, excluding some rare variants (for example, MODY, maturity-onset diabetes of the young), there is not an unavoidable transmission from one generation to the next one. What does exist instead is a family predisposition, especially in type 2 diabetes: if a first degree relative (parents, brothers/sisters) is diabetic, the risk of disease onset is higher than the one of a person with no diabetic relatives.
The main forms of diabetes are two: type 1 diabetes (with no insulin secretion) and type 2 diabetes due to reduced insulin sensitivity in liver, muscle and adipose tissue and/or a reduced insulin secretion by the pancreas.
In type 1 diabetes, pancreas can not produce insulin because the insulin-producing cells, the β-cells, are destroyed. This type of diabetes regards 3-5% of diabetic people and it has an early onset (during childhood or adolescence) but it can appear also in adults. Type 1 diabetes is then characterized by an autoimmune or idiopathic beta-cells destruction which leads to an absolute insulin deficit.
The cause of type 1 diabetes is obscure but it is now known that at the base of the disease there is an immune system “sabotage” against insulin producing cells: in fact, the pathology manifests with the appearance of antibodies against antigens found in the insulin producing cells. For this reason, type 1 diabetes is classified as “autoimmune” disease, characterized by an immune system reaction against the organism itself. The damage caused in the insulin-producing cells is believed to be linked to hereditary and/or environmental factors (for example the nutrition, lifestyle, the contact with specific viruses).
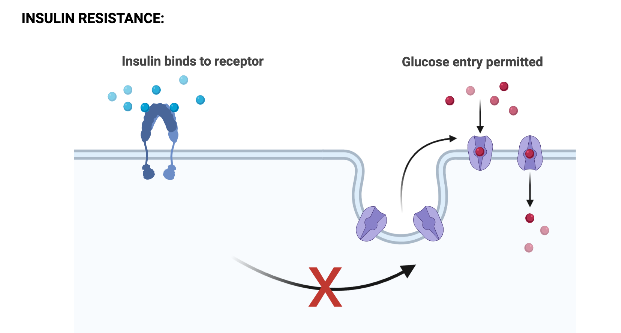
In type 2 diabetes, the amount of insulin produced by β-pancreatic cells is not sufficient or does not work: the organism’s cells are insulin resistant and do not answer to the signals of this hormone, so they prevent the entrance of glucose in cells. This causes an increase in blood glucose level, even if the organism produces larger amount of insulin to keep the glycemia under control. This condition is called insulin resistance.
Type 2 diabetes is the more frequent form of diabetes and it is typical of adult age.
RISK FACTORS:
The principal risk factors for type 2 diabetes are:
- POSITIVE FAMILY HISTORY
- OBESITY BMI ≥ 30 kg / m2
- SEDENTARITY
- ARTERIAL HYPERTENSION PA≥140 mmHg / 90mmHg
- HDL cholesterol ≤ 35 mg / dl
- TRIGLYCERIDES ≥ 250 mg / dl
The alarm signals potentially found in type 2 diabetes are:
- intense and persistent thirst (polydipsia)
- frequent need to urinate (polyuria) even at night (nocturia)
- intense hunger (voracity)
- frequent urinary infections (cystitis)
- sexual dysfunctions
The metabolic syndrome is a complex clinic condition, determined by the simultaneous presence of three conditions: diabetes, high pressure and obesity.
Since each of these conditions, considered individually is a known risk factor for the heart and blood vessels, their combination significantly increases the probability of developing cardiac issues, ictus and other vascular diseases.
Diabetes, high pressure and obesity are related to each other and they are more and more frequent in the population because of wrong habits and lifestyle. This explains the large diffusion of metabolic syndrome, which nowadays regards one adult person among 4.
Sometimes, metabolic syndrome is called “insulinresistance syndrome”, because it is thought that its principal cause is the insulin resistance.
Other conditions which seem to be involved in the metabolic syndrome onset and are still under study are:
- fatty liver (accumulation of triglycerides and other fats in the liver)
- polycystic ovary syndrome (tendency to produce cysts in the ovaries)
- gallstones
- breathing problems during sleep (such as sleep apnea)
Physiologically, insulin stimulates the synthesis and secretion of leptin.
Leptin is a peptidic hormone of 167 amino acids which is mainly produced by subcutaneous adipose tissue but also by placenta, mammal glands, skeletal muscle, stomach, pituitary gland.
Its blood levels are proportional to the fat mass; in fact, women have much higher levels compared to men with the same amount of adipose tissue. The secretion has a circadian rhythm with a peak at midnight and it can be stimulated when a carbohydrate meal is made.
The most known function of leptin is the regulation of food assumption:
- it acts on anorexigenic (satiety) neurons
- it inhibits orexigenic (hunger) neurons
It has an important role also in reproduction: it has a permissive role on puberal development, particularly women’s one, signaling the hypothalamus when energetic availability is there and so body can procreate.
Insulin and leptin act in a synergistic way in the suppression of hunger: insulin is secreted in amounts proportional to the caloric amount of the meal and the carbohydrate content; leptin is produced afterwards to potentiate the insulin anorexigenic signal on hypothalamus.
Obese people have higher levels of circulating leptin but a reduce hypothalamic sensitivity to the anorexigenic action of leptin itself, a similar effect of the one we can see in insulin-resistance.
The chronic hyperinsulinemia typical of obesity, of type 2 diabetes and of metabolic syndrome, together with the high leptin levels, causes a condition of hypothalamic resistance to the excessive leptin and an increase in the secretion of inflammatory cytokines. We can then see an activation of the immune system which worsen, like a vicious cycle, the insulin sensitivity of adipose tissue itself (fibrosis of adipose tissue, reduced uptake of glucose) and other tissues (muscle, liver).
In fact, leptin has an important immune role: it stimulates the activity of neutrophils, T cells and the secretion of inflammatory cytokines useful in the immune response and in the defense against pathogens; it also reduces adrenal activity by counteracting the secretion of cortisol.
Leptin appears to promote autoimmunity phenomena: women who have higher levels of leptin are more susceptible to autoimmune diseases.
Conversely, leptin deficiency depresses the immune system, activates the adrenal axis and inhibits the gonadal and thyroid axis.
Il diabete di tipo 2: caratteristiche, cause e sintomi
- https://www.humanitas.it/malattie/diabete-tipo-1/
- https://www.siditalia.it/divulgazione/conoscere-il-diabete#:~:text=Definizione,che%20viene%20prodotto%20dal%20pancreas.
- https://www.issalute.it/index.php/la-salute-dalla-a-alla-z-menu/s/sindrome-metabolica
- True C, Kirigiti MA, Kievit P, Grove KL, Smith MS. Leptin is not the critical signal for kisspeptin or luteinising hormone restoration during exit from negative energy balance. J Neuroendocrinol. 2011;23(11):1099–1112. doi:10.1111/j.1365-2826.2011.02144.x
- Guyenet SJ, Schwartz MW. Clinical review: Regulation of food intake, energy balance, and body fat mass: implications for the pathogenesis and treatment of obesity. J Clin Endocrinol Metab. 2012;97(3):745–755. doi:10.1210/jc.2011-2525